What is the retina?
The retina is a small patch of tissue on the back interior of your eye. This light-sensitive tissue is responsible for turning light into brain signals, which then travel through the optic nerve connected to our brain, allowing us to see what is in front of us. A healthy retina is an essential part of good vision, and any damage caused to it can be very detrimental to vision.
What is diabetic retinopathy?
Diabetic patients are prone to a disease called diabetic retinopathy. People with all types of diabetes (type 1, type 2 and gestational) are at risk. 40 to 45% of Americans with diabetes have some stage of diabetic retinopathy, and only about half are aware of it.
Poorly controlled blood sugar, or a long history of diabetes causes damage to the tiny blood vessels located on the retina. These damaged blood vessels begin to leak fluid and blood into the eye, causing blind spots and blurriness. In the most advanced stage of the disease, new abnormal blood vessels begin to grow (proliferate) on the retina, which leads to bleeding and scarring.
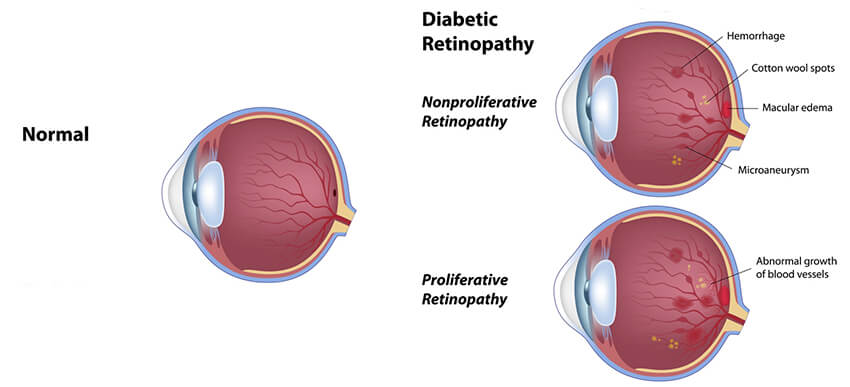
Diabetic retinopathy is a progressive disease, meaning it gets worse over time. There are two main stages of diabetic retinopathy.
- Non-proliferative or “background” diabetic retinopathy (NPDR): This is the first stage of diabetic retinopathy in which small blood vessel abnormalities (microaneurysms) and small spots of blood (“dot and blot hemorrhages”) develop. As this stage progresses, macular edema or swelling may develop which can lead to decreased vision. As this stage progresses, areas of lack of blood flow or “ischemia” may develop which contributes to the next stage of diabetic retinopathy.
- Proliferative diabetic retinopathy (PDR): In response to lack of blood flow, the retina begins to grow new blood vessels (neovascularization). Although this may seem like a healing process, these blood vessels are fragile and grow into the vitreous gel and along the surface of the retina. These blood vessels may bleed into the middle of the eye or the “vitreous cavity” and cause floaters or decreased vision. In the later stages, accompanying scar tissue can contract and pull the retina off of the interior eye lining, forming a “traction” retinal detachment.
What are the symptoms?
Generally, the early stages of diabetic retinopathy do not have symptoms. Even potentially blinding stages of diabetic retinopathy may not have symptoms and this is why it is so important that you have your eyes checked at least annually even if your vision seems fine. Symptoms that may be noticeable include blurring of vision, increased floaters or a sudden decrease in vision.
Diabetic retinopathy treatment options
The swelling associated with diabetic retinopathy (referred to as diabetic macular edema) can be treated a number of ways. Some treatments for diabetic macular edema include:
- Anti-VEGF Injection Therapy. Anti-VEGF drugs can be injected into the vitreous gel (in the middle of the eye) to block vascular endothelial growth factor (VEGF), which keeps new, abnormal blood vessels from growing.
- Corticosteroids. Corticosteroids can be injected or implanted into the eye to suppress diabetic macular edema, reducing swelling.
- Vitrectomy. A vitrectomy is a surgical procedure in which parts of the vitreous gel (in the middle of the eye) are removed. This surgery is generally used to treat the most advanced version of diabetic retinopathy.
Our diabetic eye care experts at OCLI understand that well controlled blood sugar can be difficult to achieve, especially in patients who are insulin dependent or insulin resistant. Our doctors are here to work with you to help preserve your vision. Call OCLI today to schedule your eye examination and see if your eyes require treatment.